The Impact of Diabetic Nephropathy
Diabetic nephropathy is one of the most challenging microvascular complications associated with diabetes. This condition manifests itself through kidney damage due to prolonged high blood sugar levels, ultimately leading to kidney failure if left untreated. According to recent studies, approximately 40% of individuals with diabetes will experience nephropathy at some point in their life. Understanding the causes, risk factors, and preventive measures related to diabetic nephropathy is vital in promoting kidney health and overall well-being.
We will explore the causes of diabetic nephropathy, the role of blood glucose and blood pressure, the importance of lifestyle modifications, and contemporary perspectives on prevention and management. Through this discussion, we will gain an insight into the significance of addressing diabetic nephropathy in the diabetic population.
Causes of Diabetic Nephropathy
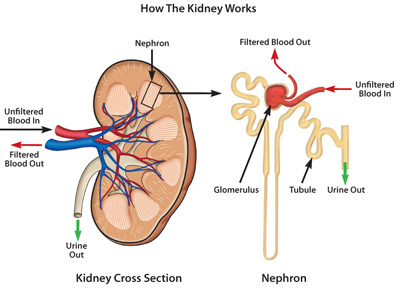
Diabetic nephropathy occurs primarily due to damage to the small blood vessels in the kidneys, which are integral in filtering waste products from the bloodstream. High glucose levels lead to a condition known as hyperglycaemia, which creates an environment conducive to vascular damage. Over time, elevated blood sugar causes structural and functional alterations within blood vessels, specifically those present in the kidneys.
Research indicates that when a person has diabetes, the kidneys go through changes that often result in an increased filtration rate early in the disease. Eventually, however, this hyperfiltration leads to further damage. The kidneys begin to scar, reducing their efficiency in waste removal and leading to a buildup of toxins in the bloodstream.
Another significant contributor to diabetic nephropathy is hypertension, or high blood pressure. Prolonged hypertension exerts excess pressure on kidney blood vessels, causing them to weaken further. When blood pressure remains uncontrolled, the risk of renal damage significantly increases, creating a vicious cycle of worsening kidney function.
Apart from hyperglycemia and hypertension, other health issues also contribute to renal disease progress. High cholesterol levels are another risk factor that can exacerbate kidney damage, leading to a greater risk of nephropathy. Cholesterol deposits in blood vessels interfere with proper circulation, resulting in reduced oxygen and nutrient delivery to renal tissues. Lifestyle factors such as smoking and excessive alcohol consumption can amplify these risks by promoting both hypertension and cholesterol issues.
Risk Factors and Vulnerable Populations
Individuals with either Type 1 or Type 2 diabetes are vulnerable to the onset of diabetic nephropathy. Those who have had diabetes for more than ten years face an even greater risk of developing renal complications. This long duration of hyperglycemia is often compounded by poor management of blood sugar and blood pressure levels. Genetic predisposition is also an important aspect, as some individuals may inherit a higher risk of kidney disease from their families.
The ethnic background plays a role in the prevalence of diabetic nephropathy. Certain populations, such as African Americans and Hispanic Americans, have a higher incidence of renal disease related to diabetes. Social determinants of health, such as access to healthcare and education regarding diabetes management, further influence these disparities, making some groups more at risk than others.
Importance of Blood Glucose and Blood Pressure Control
Managing blood glucose levels is paramount in preventing diabetic nephropathy. Regular monitoring of blood sugar and maintaining levels within an acceptable range can significantly reduce the risk of kidney damage. The American Diabetes Association recommends keeping haemoglobin A1c levels below 7 percent for the majority of adults, although individual targets may vary based on personal circumstances.
As a result with a bad glucose control, managing blood pressure is equally critical. Maintaining blood pressure levels below 130/80 mmHg significantly decreases the risk of developing nephropathy. Antihypertensive medications, particularly angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), have shown efficacy in protecting kidney function among patients with diabetes. These medications help reduce blood pressure while also providing direct protective effects on the kidneys, thereby reducing albumin excretion in the urine.
Lifestyle Modifications for Renal Protection
Lifestyle changes play a crucial role in the prevention and management of diabetic nephropathy. The first line of defence against kidney disease involves maintaining optimal blood glucose and blood pressure levels. Individuals with diabetes should follow a personalized meal plan, focusing on nutrient-rich foods that contribute to stable blood sugar levels, such as vegetables, whole grains, lean proteins, and healthy fats.
Regular physical activity is another vital component. Engaging in moderate exercise for at least 150 minutes per week can help with weight management, improve insulin sensitivity, and support cardiovascular health. These factors contribute positively to overall kidney health.
In addition to controlling blood glucose and blood pressure, avoiding harmful lifestyle choices such as smoking and excessive alcohol consumption is essential. Smoking is known to constrict blood vessels and exacerbate hypertension, increasing the risk of kidney damage. Quitting smoking can yield immediate benefits for kidney health and overall well-being. Similarly, reducing alcohol intake helps to maintain better control of blood pressure and body weight, further decreasing nephropathy risks.
Modern Perspectives on Nephropathy Management
Recent developments in the understanding of diabetic nephropathy have significantly shifted how healthcare professionals approach its management. Research into the molecular mechanisms underlying kidney injury has opened up new avenues for intervention. Medications that target specific pathways involved in kidney damage are becoming more prevalent. For instance, SGLT2 inhibitors, a newer class of diabetes drugs, not only help lower blood glucose levels but have also demonstrated protective effects on renal function and reduced the risk of heart failure in patients with diabetes.
The lifestyle interventions are receiving increased attention. Health professionals now emphasize the role of diet, exercise, and mental health in the comprehensive management of diabetes and its complications. Support groups and counselling are increasingly integrated into treatment plans, recognizing the psychological aspect of managing a chronic condition like diabetes.
As technology advances, continuous glucose monitoring systems are being utilized more widely. These devices provide real-time data on blood sugar levels, allowing individuals to make informed decisions regarding their diet and medication in an effort to maintain optimal blood sugar levels. This proactive approach represents a critical shift in diabetes care, moving toward personalized management strategies.
The Future of Diabetic Nephropathy Prevention and Care
Looking ahead, the challenge remains to reduce the prevalence of diabetic nephropathy effectively. Public health initiatives aimed at raising awareness of dia
betes management are crucial. Educational campaigns that highlight the importance of regular health check-ups and monitoring can play a vital role in early detection and intervention.
The individual-focused strategies, including tailored treatment plans for managing diabetes, will be essential. These plans should consider an individual’s unique circumstances, preferences, and comorbidities. Advances in technology and data analytics may pave the way for better predictive tools to identify those at high risk for nephropathy, enabling earlier interventions.
Diabetic nephropathy is a significant complication of diabetes that poses challenges to millions worldwide. Understanding its causes, risk factors, and the impact of blood glucose and blood pressure control is vital for prevention. Lifestyle modifications, alongside recent advancements in treatment approaches, offer hope for those at risk of developing renal disease. As we move forward, a collaborative effort among healthcare providers, patients, and communities will be essential in tackling this pressing health issue and ensuring better outcomes for individuals living with diabetes.